http://sphweb.bumc.bu.edu/otlt/MPH-Modules/PH/PH709_Cancer/PH709_Cancer_print.html
http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-what-is-cervical-cancer
http://www.proteinatlas.org/dictionary/cancer/cervical+cancer/detail+1
http://www.cap.org/apps/docs/reference/myBiopsy/cervicalsquamous.pdf
http://www.histology-world.com/photoalbum/displayimage.php?album=39&pid=1538#top_display_media
Histology: Cervical Cancer
Tuesday, April 29, 2014
Diagnosis and Treatment
It is hard for someone to tell if they have cervical cancer
or not because in pre-cancers, there are usually no symptoms. It isn’t until
the cancer has progressed enough and has moved into nearby tissues that there
are finally symptoms. This is usually when someone would go in to see their
doctor, and this usually means you’re in past stage I.
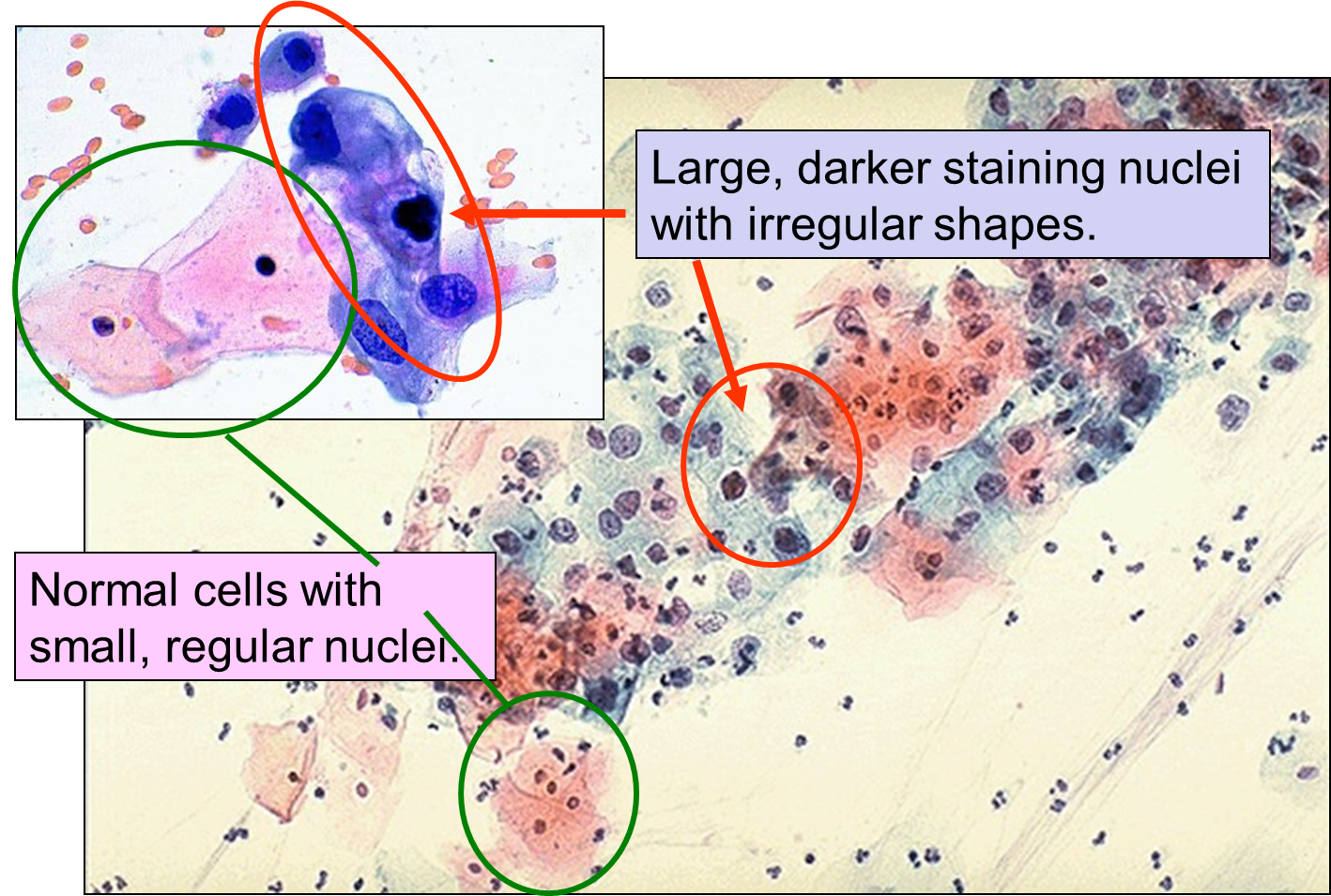
Now, doctors suggest getting tested, and the first step is getting regular Papanicolaou, or Pap tests. The Pap test looks for any abnormalities in the cervical cells. The
normal squamous epithelial cells are pale blue to orange in color and are
plate-like. The cancerous epithelial cells will look smaller overall, with
darker and more irregular nuclei.
If the Pap test shows the abnormal epithelial cells, then your doctor will want to do a colposcopy. This is a procedure that allows the doctor to examine the cervix with more detail and actually see if there are any irregularities on the cervix. A colposcope is the instrument that they use. It uses lens like a binoculars to zoom in on the cervix.
 |
| This picture is showing both a normal cervix and one that has some abnormal growth. |
Once they have examined the cervix, they'll do a biopsy if they see any irregular growth on the cervix and remove a small piece of tissue to run tests.
Cervical Cancer Stages
 |
| This shows the regions for each stage of cancer. |
There are five stages of cervical cancer,
starting at 0 and progressing to 4, with each new stage getting more severe.
The first stage is 0. This means that the cancer cells are found on the surface
of the cervix, and nowhere else. When the cancer has localized to the cervix,
it’s a stage I cancer. In stage II, the cancer has spread up the cervix and
into the upper part of the vagina. When it reaches the lower part of the
vagina, it’s a stage III cancer. Stage IV is very severe and has spread from
the cervix and vagina into the bladder and/or rectum. It could even progress
into the lymph nodes and lymphatic vessels.
 |
| This is the anatomical progression of cervical cancer. |
 |
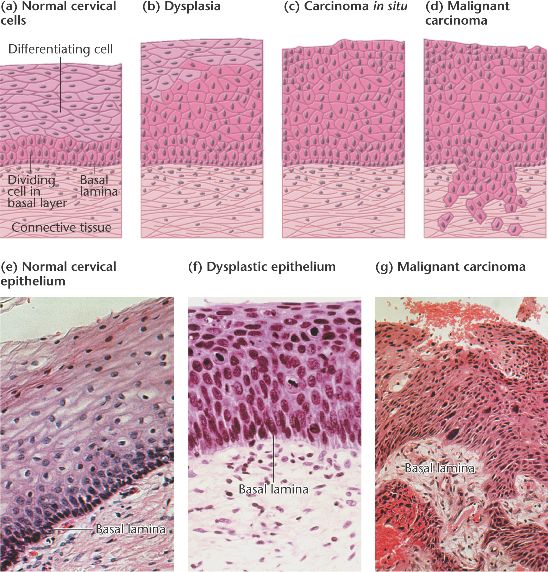
| This is a diagram of the progression of the cancer. Notice how the cells and the nucleus become irregular in shape. |
Cervical cancer may spread to the bladder, intestines, lungs, and liver. Often there are no problems until the cancer is advanced and has spread. Symptoms of advanced cervical cancer may include:
- Back pain
- Bone pain or fractures
- Fatigue
- Leaking of urine or feces from the vagina
- Leg pain
- Loss of appetite
- Pelvic pain
- Single swollen leg
- Weight loss
Treatment
The treatment of cervical cancer greatly depends on which stage of the cancer you are in and is therefore based on the individual circumstance. Age, overall health, quality of life, and the desire to have children are all factors that people have to look at in their own predicament. With that being said, there are different treatment choices one can make to try and eliminate the cancer.
- Surgery
- Radical Trachelectomy
- This procedure is fairly new. They can now remove the cervix and part of the vagina, and then connecting the uterus to the remaining part of the vagina. This allows people to still have children, which is important because most women have cervical cancer around the age of 30.
- Radiation Therapy
- This is the use of high-energy X-rays to kill cancer cells in a targeted area.
- Chemotherapy
- This is the use of drugs to reach the cancer wherever it is in the body.
- It targets cells that divide rapidly, anywhere in the body. This can be risky because there are other cells besides cancer cells that divide rapidly. i.e. cells in the bone marrow, digestive tract, and hair follicles.
- Chemoradiation Therapy
- This is the combination of radiation and chemotherapy.
Glossary
Apoptosis: A form of programmed cell death.
Epithelium: The epithelium, or epithelial tissue, is tissue that covers the external surface of the body and lines hollow structures inside the body.
Neoplastic: A new, often uncontrolled growth of abnormal tissue; tumor.
Oncogene: A gene that encodes a protein that can bring about cell transformation (usually in combination with other oncogenes).
Transcription Factor: A protein that binds to a regulatory element and thereby directly or indirectly affects transcription of a gene or group of genes.
Transformation: The series of changes that a normal cell undergoes as it becomes malignant.
Tumour Suppressor: A gene encoding a protein that suppresses (inihibits) tumour formation. These genes normally prevent unlimited cell division.
Monday, April 28, 2014
Histological Findings
Cervical cancers and pre-cancer types are determined
by certain features found under the microscope. When determining which kind of
cervical cancer it is, they look at two cell types, the squamous epithelial and
the glands. If the cancer is in the epithelial lining, then the cancer is called
Squamous Cell Carcinoma. If it is in the glands, then it is called Adenocarcinomas.
Usually it is Squamous Cell Carcinoma, about 80-90% of the time. This type
often occurs in the transformation zone, or where the exocercix joins the
endocervix.
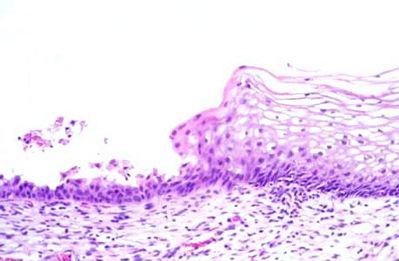 |
| This picture shows the transformation zone. On the left is the Endocervix, with the columnar epithelium, and on the right is the Exocervix, with the nonkeratinized stratified squamous. |
 |
| In this example of Squamous Cell Carcinoma, you can see the abnormal growth in the transformation zone, where the exocervix and the endocervix meet. |
 |
| Adenocarcinoma |
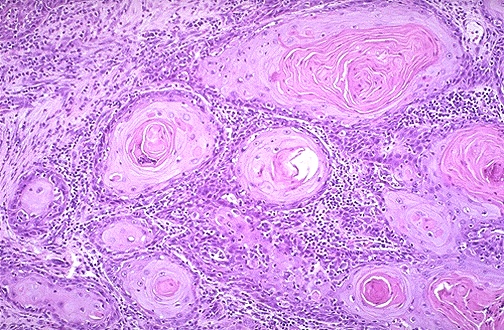 |
| At high magnification, nests of neoplastic squamous cells are invaded through a chronically inflamed stroma. It is poorly-differentiated. |
 |
| Squamous Cell Carcinoma |
Friday, April 25, 2014
Introduction
Like any form of cancer, there isn’t one sign that
someone will get cervical cancer 100%. However, there are risk factors that
increase the likelihood of someone developing cervical cancer. The most
influential of all the risk factors is Human Papilloma Virus (HPV). Certain
types of HPV are referred to as high-risk types because they are strongly
linked to cancers; in fact more than 99% are caused by these high-risk HPV
viruses. High-risk strains 16 and 18 cause 70% of all cervical cancers. Along
with HPV, smoking, Human Immunodeficiency Virus (HIV), oral contraceptives, and
pregnancy at a young age are also risk factors. Having more than one of these
factors greatly increases your chance of developing cancer of the cervix.
 The cervix is the thin, lower portion of the uterus and is
conjoined to the top of the vagina. There are 2 main types of cells that cover
the cervix, stratified squamous cells, which are on the exocervix, and mucus-secreting columnar epithelium, which are on the endocervix. The transformation zone is where these two types
of cells meet and is where most cervical cancers start.
The cervix is the thin, lower portion of the uterus and is
conjoined to the top of the vagina. There are 2 main types of cells that cover
the cervix, stratified squamous cells, which are on the exocervix, and mucus-secreting columnar epithelium, which are on the endocervix. The transformation zone is where these two types
of cells meet and is where most cervical cancers start.HPV encodes for the production of the viral oncoprotein known as E6. This turns off some of the tumor suppressor genes. The high-risk HPV E6 proteins can associate with the p53 tumor suppressor protein by binding to it through transcriptional modulation. This interaction promotes the degradation of p53 in vitro, which presumably accounts for the very low levels of p53 in cervical carcinoma cell lines. Normally, the p53 gene would initiate apoptosis of a cell with the mutant DNA. Below you can see the effects when the high risk HPV is present.
 |
| This is the gross appearance of stage I cervical squamous cell carcinoma |
Subscribe to:
Comments (Atom)